June 22, 2023
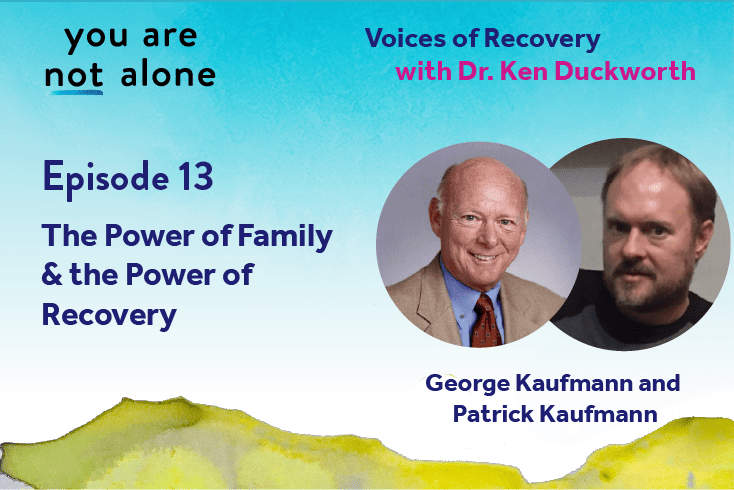
George Kaufmann, a father, and Patrick Kaufmann, his son, have developed some incredible communication skills as their family has come together around Patrick’s mental health condition. In a broad-ranging conversation with NAMI’s Chief Medical Officer, Dr. Ken Duckworth, George and Patrick recall Patrick’s struggle with substance use disorder and schizoaffective disorder, how the family learned the best and most effective ways to support him, and what they learned about their family culture. They also discuss Patrick’s involvement with NAMI as a Peer Support Specialist.
This conversation was part of Dr. Duckworth’s research for the book, You Are Not Alone: The NAMI Guide to Navigating Mental Health–With Advice from Experts and Wisdom from Real People and Families. Hear more episodes of this and other podcasts at nami.org/podcast.
[0:00] [background music]
Narrator: [0:00] This is "You Are Not Alone ‑‑ Voices of Recovery."
Dr. Ken Duckworth: [0:04] Hi. I'm Dr. Ken Duckworth. I'm a psychiatrist and the chief medical officer for NAMI, the National Alliance on Mental Illness. I'm the author of NAMI's first book, "You Are Not Alone ‑‑ The NAMI Guide to Navigating Mental Health ‑ With Advice from Experts and Wisdom from Real People and Families."
[0:21] I talked to over 100 people for this book. I wanted to share some conversations that I found could be helpful to us all. In a conversation with George Kaufmann, the dad, and Patrick Kaufmann, his son, I found some remarkable moments of how they learned to communicate around Patrick's mental health condition.
[0:45] This family has been central to Patrick's recovery. The idea of a family also meant a great deal to Patrick. The family is originally from Kalamazoo, Michigan although George and his wife, Patrick's mom, later moved to California.
Patrick Kaufmann: [1:04] The thing that gave me hope was remembering my family. My parents got involved in NAMI. They had their recovery. I think parents have recovery, too.
[1:19] I didn't know what recovery was, really. I might have heard them talk about it. I didn't really pay much attention. It was something in the back of my mind that, when the right time came around, I thought, "My parents are over there doing something good. They've got some kind of hope in their lives. Maybe, I can do that, too."
[1:40] The other piece of that was I always wanted to have a family of my own. When I started having schizophrenia, I was 18. I wasn't diagnosed till 19 or 20. One of my things that was going on was a delusion that I had that I would marry this girl that I met at school.
[2:02] I'd only had one class with her, and she moved on to Princeton. That was the end of it, but I thought I was going to track her down, marry her and have kids with her. I had all these kids in my head. I had them all named. I had middle names. I talked to them all the time, their personalities, the whole nine yards.
[2:21] I was so stuck on that because I invested so much in it. I mean, that was my future. Every day that went by, I was investing more of my attention into this family I thought I was going to have.
[2:32] There was a point where, I didn't completely write it off, but I realized I'd been waiting for 10 years for this to happen, maybe it's not going to happen, so what's next?
[2:46] That was the point where I thought, maybe I'll try something new and see if I can start a life from here. Part of that was wanting to have a family and starting to believe that maybe I could do something in the real world.
Dr. Duckworth: [3:02] Was there anything that happened that helped you think differently? Was it your parents, recovery? How do you make sense of it, Patrick?
Patrick: [3:11] Well, first of all, the world had to have enough value for me to believe I could get to where I wanted by walking there rather than just dreaming outside of this world, something so far away that is unattainable, but believing somehow I'll fly there and get there.
[3:30] Believing that the moment I was in had enough value that I could do something with it. Some of this was my parents, but they would let me talk about it and question it openly. Instead of saying, "That's all nonsense, get it out of your head," they started to get where they would listen to me talk about it.
[3:55] They might say things like, "Wow, that sounds like a really cool family." I don't use the term "delusion" too much because sometimes it doesn't apply, but them letting me have that conversation. I remember saying, "They're like stars in the sky, Dad." He's like, "That's really cool. That has meaning to you."
[4:20] I think being able to think that way brought me down a little bit more to where I could talk about it and think about it and maybe challenge it a little bit. Then I had a psychiatrist that I said, "Is this real? Is it possible that this is real because it's still in my mind?" I had told him all about it.
[4:40] He looked at me, he said, "It's not likely." That was much better than saying, "There's no way it's true. It's impossible. Good luck, it's not going to happen." He just said it's not likely, and that made me feel like, "OK…" It made it to where I could think about it logically and think, "This probably isn't going to happen." It was safer to approach it that way than to be like, "I got to force it out of my head."
Dr. Duckworth: [5:05] Both your parents and the psychiatrist came alongside of it, instead of saying to you, "What you're thinking is wrong or not real," they were open to thinking about it with you. Your parents approach it differently than the psychiatrist, but, "Let's talk about it. Let's try to understand that."
[5:25] George, did you get that strategy from NAMI classes, or is that just your natural heart? That is a heart intervention, not every parent can do that.
George Kaufmann: [5:37] What Patrick is talking about happened about eight or nine years in. We did what most families do. First thing we do is we try to fix it, and all that does is push the person further away. We had eight years to find out what didn't work, and by process of elimination and partly by that time we were well connected with NAMI.
[6:05] By that time, we were around other people who have had similar experiences, and we shared a lot about what didn't work. We're able to then move on. By that time, there were the family‑education classes and everything. That was probably somewhat a part of it.
[6:25] A lot of it was just our basic experience of banging your head against the wall and having the same outcome of it not working. The more that we would focus on mental illness, his symptoms, his treatment, or compliance, the more it pushed him away. It's amazing how long it can take smart people to get that message.
[6:50] [laughter]
George: [6:50] Not that we're brilliant, but after a while, you do. Then, you begin to realize that the trick of all of this above everything else is to treat every person with the same respect that you would like to get. When you do that, it builds trust. As you build that trust, the walls come down.
Patrick: [7:21] I went to a conference with my dad. Was that before I even got clean? Do you remember the first conference we went to?
George: [12:51] Probably.
Dr. Duckworth: [14:38] Is this a NAMI conference or a different conference?
Patrick: [4:39] It was probably NAMI, wasn't it, Dad? Do you remember?
George: [7:36] It was NAMI.
Patrick: [7:39] Just hearing from other people, there was people that had the same experiences as me, hearing voices from the TV or whatever it was, and they were getting their doctorates. I was so amazed by that. That was my first experience knowing that.
[7:58] What the system had told me is, "You're mentally ill. You don't have to work, maybe you shouldn't work. Don't expect anything different. You just got to survive this. There you go." That was pretty inspiring.
[8:13] I also had a guy in a…What would I call it? Maybe a halfway house. It was kind of an adult foster care, but it was more independent living. There was for substance abuse, too. It was for cocaine.
[8:28] Actually, this is another piece of the so‑called delusion part because I told him about it, and he said, "Maybe it's another dimension." That helped me put it in perspective, too. Maybe it's not in this world. That was helpful even though that was a little more out‑of‑the‑box response.
[8:47] He was the first person I met that had some of the same background as me like the substance abuse and everything and had found that life was still worth living without drugs. That wasn't something that I fully grasped yet that you could actually be happy and have fun because I thought you always need drugs for that.
[9:09] Seeing someone like that who is a year into recovery and had the same thinking as me. Some of us are critical about the world like the world is a bad place, the environment, the poverty, everything else. He was someone who actually thought about things like that, didn't ignore them, but still was able to find happiness.
Dr. Duckworth: [9:31] That's how you set the substances down. How big a piece of your recovery was that?
Patrick: [9:39] I guess I would say half.
Dr. Duckworth: [9:41] Half.
Patrick: [9:44] I'm sure you've heard it before where people say the substance abuse feeds off the mental illness, but then it's vice versa, too. As I got into recovery from drugs, my mental health improved. As my mental health improved, it was easier not to get into the drugs.
George: [10:01] Right.
Dr. Duckworth: [10:02] Do you credit up the program? Sounds like it was also helpful to you.
Patrick: [10:06] Actually, the substance abuse program I had started before I quit using…It was the kind where you can attend, it was harm reduction, you didn't have to quit. They didn't give you a hard time or anything. That planted the seed to where I knew, "I can do this if I choose to, and I know some of the skills," and then I came back to it later and did the group again.
George: [10:29] His particular county mental health department, it was amazing to me. When he did make the decision, there was a moment that he decided, that you wanted to get clean and sober, they immediately found a bed for him in a six‑bed residential dual‑diagnosis center [indecipherable] about, with a single team treating both the mental health issue and the substance abuse issue.
[10:54] Told him he could stay there and live as long as he wanted there, until he could go on the outside without using again. You were there about six months, I think, right?
Patrick: [11:03] Six months.
George: [11:04] Anyway, that was a…
Dr. Duckworth: [11:04] That is not common. You got a fortunate opportunity.
Patrick: [11:13] It was essential, too, because no matter how strong I was in my recovery, the place I was living before I went into the drug treatment place where you just get clean, before I moved out into the living place, the place I was living before that was…It was basically a crack house. There was people showing up to get drugs.
[11:38] I tried to quit, and someone kicked my lock, kicked my door in. People were walking in and they would have drugs right there. It was hard to say no. Between the time I decided to quit and got into treatment, there was a few days that I ended up using again, even though I had gotten excited about it. You got to get out of that environment before you can really quit.
Dr. Duckworth: [12:01] George, tell me about your parental experience. You have this education process through Family‑to‑Family, where you realize you can just go back to loving him and talking with him about his experience. Do I characterize that properly?
George: [12:19] That's the idea, you try to do that, but the other thing that you learn in this process is that it's never a linear path. There were periods where we were hopeful and encouraged that Pat was making progress. Just like he said, it was back and forth for a while and up and down.
[12:41] Now, I'm not sure, and Pat will have to explain how he came to accept treatment for the mental health piece of it, it seemed to me like it happened when you were living out here with us that brief time. He began to finally accept treatment for the mental illness, but he was still using for a period of time.
[13:05] What we saw at that point was that he was markedly different. Much improved, but still sort of in a fog sometimes, to people and engaging with other people.
[13:22] Once he got to that point that he just described, where you finished that six months, or whatever it was, in the residential facility and came back out into the community, it was like, here was this wonderful, caring, sensitive young person that we hadn't seen in that whole subsequent 10 years.
Narrator: [13:46] Patrick chose to leave California and returned to Michigan to continue his recovery journey.
Dr. Duckworth: [13:52] Patrick, so old are you now, may I ask?
Patrick: [13:55] 46.
Dr. Duckworth: [13:56] 36?
Patrick: [13:57] 46.
Dr. Duckworth: [13:58] 46. You've been in a recovery zone for a decade and a half, perhaps, or more?
Patrick: [14:08] Yeah, a little more.
Dr. Duckworth: [14:07] A little more?
Patrick: [14:10] 17 years in May.
Dr. Duckworth: [14:11] Fantastic. Have you had, as you look back on it, sounds like there were some key things that happened in there. Was the family letting go and supporting you to go back to Michigan one of them?
Patrick: [14:26] Bigger than that. I didn't notice what was going on at that time, if that was a process for them or anything. I just wanted to go back and I did. The idea of letting go was important because, I don't know if this makes sense, but if somebody's drowning and you're in a boat and you jump in to save them, you end up drowning each other.
[14:56] Feeling like they were jumping in with me and they were going to drown with me, didn't help anything. Knowing that they were OK made a difference, not feeling like every decision I made was going to affect them so deeply, because it was painful to feel like somebody was that invested in you and you didn't feel able to care enough for yourself to make them happy.
Dr. Duckworth: [15:27] As the burden lifted, you made the psychological leap to realize that they would be OK, and you had to rescue yourself from drowning?
Patrick: [15:48] Yeah, because once they were OK and taking care of themselves, it instilled independence, because it was like them having faith that…I guess, if you use that scenario, if you continue to use it, maybe once I stopped panicking, it was easier to just float there and then swim ashore or whatever. It made me feel like they believed I could do it, when they stopped being so…trying to rescue me.
Dr. Duckworth: [16:26] It requires a big leap on all parties' part.
George: [16:32] I remember one time, you were giving a talk somewhere and somebody asked you a question about that, and the way that you answered it, I thought it was cool. He said, "When they were hovering over me, 'Are you OK? Are you feeling OK?' 'Yeah.' 'You seem angry.'" [laughs] It was like, we didn't really believe that he could get better.
[16:53] When we backed off and went on with our own lives, he said, "The message that I got was that, 'Huh, maybe they really think I can get better.'"
[17:03] Of course, we didn't have any sense of that whatsoever. Our whole idea for the first 10 years was just to try to keep Patrick alive. That was the big goal for us because we didn't know what he was…or anything about mental illness or what he was doing or choices he was making or anything, and some of them were potentially dangerous.
Narrator: [17:30] As Patrick's recovery continued and strengthened, and his involvement with NAMI deepened, he became a peer support specialist.
[17:39] Peer support specialists are individuals with lived experience of recovery from a mental health condition, a substance use disorder, or both, and are trained to support other individuals and families in their recovery, with the cornerstone being the knowledge that they know what it's like to walk in your shoes.
Dr. Duckworth: [18:01] Patrick, when did you become a peer specialist, and what was that like for you?
Patrick: [18:11] I don't know the year. Actually, I think it was 2005, but being a peer support was one of the things that made recovery seem possible because I had no job resume and no skills that I could really think of.
[18:33] Even if I got clean and did something good with my life, started feeling better, I still would have had to start at a minimum‑wage job, and being 10 years behind everybody else would've taken a lot to work my way up from there.
[18:52] That was a pretty discouraging situation, so the thing I latched onto was the peer support job. The pay wasn't bad for an entry‑level job, although I don't know what you call entry level, because technically you have life experience, but that's what I held onto.
[19:12] The substance abuse group I was going to, the peer support on that team, I talked to him and I was like, "Wow, you've got the perfect job. You get to hang out with people, tell them about your recovery, get them excited, and get paid for it," so I stalked that job. I just hovered over it till that guy quit.
[19:36] I tried to build my resume for a year. It took me about a year to get into the job. I started volunteering places, doing whatever I could to get it in place. That was the magic, to suddenly feel like I had something of value.
[19:50] Also, I haven't talked about it much, but I was really angry with the mental health system.
Dr. Duckworth: [19:55] Of course.
Patrick: [19:56] This was a way to create some positive change out of my experience and to be involved with the system, but have a positive influence on it rather than…
Dr. Duckworth: [20:07] Nice. That's great. Let me take a new paragraph. What's your family culture, religion, framework, and how does that impact any of this, or does it?
Patrick: [20:24] We're talking about my nuclear family or…?
Dr. Duckworth: [20:27] No. When you were younger, when you were a kid…
Patrick: [20:30] I got you.
Dr. Duckworth: [20:31] 18, 17, 16, what's your religion, family culture? I've talked to a lot of families who had to overcome cultural things to seek help or to recognize the challenge. Was that part of your experience, Patrick?
Patrick: [20:49] No. Maybe the opposite a little bit. My mom was always, I guess she was an activist in her younger years. This comes because with some of the civil rights stuff, right, Dad?
George: [21:00] Mm‑hmm.
Patrick: [21:02] She was that kind of thinker. I had a little bit of freedom to think outside the box. Some examples of my mom's influence could be that she told me about artists that had mental illness. That was already there in my head, so I didn't immediately think, "I have mental illness, so I'm lost to the world."
Dr. Duckworth: [21:25] That was before the onset of symptoms or as you were having symptoms?
Patrick: [21:29] Before.
Dr. Duckworth: [21:30] Before?
Patrick: [21:31] Yeah.
Dr. Duckworth: [21:31] It's super open‑thinking culture in the family.
Patrick: [21:37] On my mom's side.
George: [21:38] [laughs] No. Not on my side.
[21:40] [laughter]
Patrick: [21:43] I'm not sure what my dad would have said about mental Illness, but they were blindsided when it happened to me, because it was just so extreme and so something they had never seen.
Dr. Duckworth: [21:54] That happens all the time, Patrick. It's the rare family that has any prep at all. People get blindsided by this and they feel like they're drowning. That's one of the reasons that programs like NAMIs Family‑To‑Family and the Peer Culture are so powerful, because you actually not alone, but you do feel like you're alone. You feel like you're on an island.
[22:20] George, may I ask? When you grew up, did you have a strong religious background or what were you taught about mental health as a younger man?
George: [22:31] Not particularly. We weren't a particularly practicing religious family, although we did go to church when the kids were being raised. It was a part of our culture, but not [indecipherable] .
Dr. Duckworth: [22:46] What church did you attend?
George: [22:49] Episcopalian, at that time.
Dr. Duckworth: [22:50] Episcopalian.
George: [22:51] My wife, Millie, her godfather again, who also had married us was an Episcopalian priest, so we didn't have any choice in that. Anyway, and that was fun. We stuck with it. It was a good experience for the family, I think.
[23:06] The other thing that Patrick's not mention is that culture‑wise, we're the old‑time, command‑and‑control kind of family, where the father was in charge and mom was this…It was the old‑time approach, which wouldn't be what happened today.
[23:26] I traveled a lot over the course of my kids younger…all their years growing up, really. It fell to Mom to be the whole family during the week, and I was there on the weekends. That was not helpful. It was also not helpful that I had zero insight not only about mental illness, but about a lot of other things that actually…
[23:56] It sounds weird to say, but my life has been drastically enriched by having mental illness in the family. It sounds weird to some people.
Dr. Duckworth: [24:09] I've heard other people say that.
George: [24:11] It's really true.
Patrick: [24:12] Very [indecipherable] .
George: [24:13] It gave me a perspective that I had never had before. I think in a lot of ways. I probably pushed Patrick and his brother away at a time when they probably could have used the support the most. To their credit, both of them have since forgiven me. Actually, when it comes to the understanding and all of the mental illness, Patrick has been my greatest teacher more than anything else.
Dr. Duckworth: [24:48] Yes, of course.
George: [24:49] When I was able to finally shut up, listen to him, hear him, and not be judgmental about what I was hearing. It was a pretty slow process for me, but one that I'm glad happened. Patrick could pull me up short. He's not above telling me that I'm all [indecipherable] with him.
[25:25] I still see today, the interesting thing is that when everything's going fine, I can keep my composure and my balance. When we're under stress, we tend to revert to the way we used to be. Maybe it's a part of human nature. I don't know. Patrick has been the one that's more than anything else helped me figure out what it is that I can tell other families that might be helpful.
[25:59] In fact, one of the great things about our relationship is…We talked about this stuff. Recently, we're having, I wouldn't say an argument, but a debate about assisted outpatient treatment, an involuntary treatment, is there ever a place for that or not? That sort of thing I really listen carefully.
Dr. Duckworth: [26:23] Patrick, do you have a take on being your dad's greatest teacher?
Patrick: [26:29] I feel like he does in the way that it improved things for us. I was diagnosed in high school with depression. Schizophrenia was the thing that threw things off.
[26:42] At that time, I was really unhappy with the way my dad lived his life. He was a businessman. I would share with him ideas about social‑problem‑type stuff, and it didn't go over. I took one of those tests and it said, "Be a social worker." I was like, "No, I got to be a businessman like my dad."
Dr. Duckworth: [27:06] That was a family culture.
Patrick: [27:09] Then, I was even conscious of it that I wanted to change that he was that kind of person, that was your stereotypical businessman that just wants money and that kind of thing. Obviously, it's more complex than that, but at the time, that's how I saw him.
[27:29] I wanted to change that, and it turns out that's what happened. He's someone who volunteers all kinds of time and expertise to all these programs. I couldn't have imagined anything greater for my dad. It was actually the thing I wanted, and it turned out to happen.
George: [27:50] Way back when it took a circuitous route.
Patrick: [27:54] It took about 20 years.
Dr. Duckworth: [27:55] Patrick, who was the first person who told you that the concept of recovery was a real concept? How old were you at that point?
Patrick: [28:04] Maybe 29.
Dr. Duckworth: [28:04] 11 years in?
Patrick: [28:10] Oh, let's see. Maybe 9, 10 year with illness. I think my parents alluded to it. It seemed like something I had heard before. I don't know. They could've talked to me about it directly, but I blocked it out. I didn't want to talk about it, but it was there. Once it came up again, I was like, "Oh, yeah. This is what my parents talked about."
[28:40] Then, I got into this little program. It was a group of peers… or people with mental illness, they weren't peer supports. They would go around and talk to nursing students. That was their job. They would go and they would tell their story. That was before I quit using, wasn't it, Dad, that I got into [indecipherable] group?
George: [29:02] Right about the same time, I guess.
Patrick: [29:04] At the same time.
Dr. Duckworth: [29:05] Was that the first person who gave you the idea that there was recovery or possibility of recovery?
Patrick: [29:11] Yeah. It was a gradual realization, though. They weren't peer supports. They weren't working full‑time and building a future. They were people who were getting into this idea of, "Share my story, and it can help other people." It was a little progressive, but it was more gradual.
[29:36] The moment that recovery hit me was when I went to my first NA meeting. You know how much the two are intertwined, the substance and the mental illness. That was when I first realized how joyful I could be if I understood this concept of recovery. It was one and the same as the mental illness.
Dr. Duckworth: [30:00] Can I ask, are you taking any treatment now? Do you have a psychotherapist?
Patrick: [30:05] I just started seeing a therapist. I've seen them twice so far. Just something I'm trying out, not sure how I feel about it yet. I have a psychiatrist. That's it.
Dr. Duckworth: [30:22] What treatments, may I ask, do you take now?
Patrick: [30:26] For medications.
Dr. Duckworth: [30:27] Medications, therapy, groups, anything that you do. Have you been to an NA meeting in a long time?
Patrick: [30:35] Not really.
Dr. Duckworth: [30:37] Not really, so that's out of your life.
Patrick: [30:39] I go a couple times a year, maybe at the most.
Dr. Duckworth: [30:42] Do you take medications, and are they helpful to you?
Patrick: [30:47] I'm convinced I need the medications. I've gone off them a couple times and felt like I was doing OK. Well, that's not true. When I went off from with my parents, I realized how bad I was.
[31:06] I guess I had gone off from before I started seeing my wife. She told me I was off. Things weren't right with me. I was like, …
NAMI HelpLine is available M-F, 10 a.m. – 10 p.m. ET. Call 800-950-6264,
text “helpline” to 62640, or chat online. In a crisis, call or text 988 (24/7).